MEDICINE CASE DISCUSSION
This is an E-log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence-based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed .
I have been given this case, in an attempt to solve and understand the topic of "Patient's clinical data analysis”. This has helped me develop my competency in reading and comprehending clinical data including history taking, clinical findings and investigations. The goal is to come up with a diagnosis and treatment plan.
45 year old male patient presented with Acute pancreatitis.
This is a case of a 45 year old male, carpenter by occupation came to OPD with chief complaints of:
1. Constipation since 3 days
2. Pain in abdomen since 2days
3. Vomitings since 2 days.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 2 days ago then he developed pain in the abdomen- in epigastric region.
It was sudden in onset, gradually progressive.
Pain more after eating food and on lying in supine position.
Pain relieved on sitting , on bending forward.
-H/O 3 episodes of Vomiting yesterday after eating food, food as content, non bilious, non projectile, not blood tinged.
-Constipation since 3 days
No H/O fever, cough, cold, shortness of breath, loose stools, giddiness.
Last binge of alcohol consumption 2days ago.
PAST HISTORY:
H/O similar complaints 2 years ago- diagnosed as Acute pancreatitis, treated at KIMS Narketpally
Not a K/C/O DM, HTN, TB, Asthma, Epilepsy,CVA,CAD
PERSONAL HISTORY:
He is a carpenter by occupation
Diet - mixed
Appetite - normal
Sleep - adequate
Bowel and bladder regular
Consumes 2quarters of alcohol/day.
FAMILY HISTORY:
Insignificant
GENERAL EXAMINATION:
Patient is conscious , coherent and cooperative. Well oriented to time place and person.
No signs of pallor, icterus, cyanosis, clubbing, lymphadenopathy, edema.
VITALS:
Pulse - 76 bpm
BP - 110/80 mm Hg
RR - 18 cpm
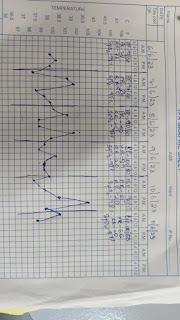
Temp- 97.8F
SpO2- 98% on room air
GRBS- 124mg%
SYSTEMIC EXAMINATION:

P/A:
Inspection:
Round, large with no distention
Umbilicus: Inverted
No visible pulsation,peristalsis, dilated veins and localized swellings.
Palpation:
Soft, tenderness present in epigastric region
No signs of organomegally
Percussion:
No fluid thrill, shifting dullness absent
Auscultation:
Bowel sounds heard 2-3/ minute
CVS:
Inspection:
There are no chest wall abnormalities
The position of the trachea is central.
Apical impulse is not observed.
There are no other visible pulsations, dilated and engorged veins, surgical scars or sinuses.
Palpation:
Apex beat was localised in the 5th intercostal space 2cm lateral to the mid clavicular line
Position of trachea was central
.
Auscultation:
S1 and S2 were heard
There were no added sounds / murmurs.
RESPIRATORY SYSTEM:
Bilateral air entry is present
Normal vesicular breath sounds are heard.
CNS:
HIGHER MENTAL FUNCTIONS-
Normal
Memory intact
CRANIAL NERVES :Normal
SENSORY EXAMINATION
Normal sensations felt in all dermatomes
MOTOR EXAMINATION
Normal tone in upper and lower limb
Normal power in upper and lower limb
Normal gait
REFLEXES
Normal, brisk reflexes elicited- biceps, triceps, knee and ankle reflexes elicited
CEREBELLAR FUNCTION
Normal function
No meningeal signs were elicited
INVESTIGATIONS:
8/4/23
Hemogram:
Hb-16.3 gm/dl
TLC-14100 cells/cu.mm
PLT- 2.16 lakhs/cu.mm
RBC- 5.18 million/cu.mm
CUE:
Albumin- +
Pus cells- 3-4
Epithelial cells- 2-3
Blood urea- 36mg/dl
Serum creatinine - 1.0mg/dl
LFT:
TB- 1.17mg/dl
DB- 0.26mg/dl
SGOT- 45IU/L
SGPT- 41IU/L
ALP- 166IU/L
TP- 6.9 gm/dl
Alb- 4.3 gm/dl
A/G- 1.67
Electrolytes
Na-140
K-4.1
CL-102mmol/l
Serum amylase- 841
Serum lipase- 218
FBS-121mg/dl
ECG-
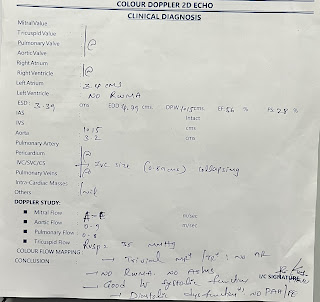
2D ECHO-
USG ABDOMEN-
CHEST X RAY
RANSONS CRITERIA
on admission
1. WBC >16,000/MICROLITRE-0
2.Age>55 yrs- 0
3. Glucose >200 mg/dl-0
4. AST>250 IU/L-0
5. LDH>350IU/K
BISAP SCORE
1. BUN>25-0
2. Impaired mental status-0
3. SIRS-1
4. Age>60-0
5. Pleural effusion- 0
SIRS
Two or more of the following criteria
1. Heart rate > 90
2. Temp > 100.4°F (38°C) or < 96.8°F (36°C)
3. Respiratory rate > 20 or PaCO2 < 32 mm Hg
4. WBC > 12,000/mm³ or < 4,000/mm³, or > 10% band forms
9/4/23
Hemogram:
Hb: 15.6 gm/dl
TLC: 11,500
Plt: 1.87
RBC: 4.94
Na- 135
K- 3.5
Cl-102
Sr creatinine -0.8 mg/dl
Lipid profile:
Total cholesterol:185
Triglycerides:130
HDL:52
LDL:108
VLDL: 106
10/4/23
Hemogram:
Hb: 16.7 gm/dl
TLC: 10,300
Plt: 1.98
RBC: 5.42
Na 140
K 3.9
Cl 102
Sr creatinine: 0.9
BUN: 29
Total bilirubin: 2.24
Direct bilirubin: 0.42
SGOT: 102
SGPT:138
ALP: 158
PROVISIONAL DIAGNOSIS:
Acute Pancreatitis.
TREATMENT:
1.NBM TILL FURTHER ORDERS
2.IV FLUIDS 1Unit NS BOLUS @100ml/hr
2 units NS, RL, 1Unit DNS
3.INJ TRAMADOL 1amp in 100ml NS IV over 1hr/BD
4.INJ THIAMINE 1amp in 100ml NS IV/BD
5.INJ PAN 40mg IV/OD
6.INJ ZOFER 4mg IV/TID
THEORY:
BISAP SCORE
1. BUN>25-0
2. Impaired mental status-0
3. SIRS-1
4. Age>60-0
5. Pleural effusion- 0
SIRS
Two or more of the following criteria
1. Heart rate > 90
2. Temp > 100.4°F (38°C) or < 96.8°F (36°C)
3. Respiratory rate > 20 or PaCO2 < 32 mm Hg
4. WBC > 12,000/mm³ or < 4,000/mm³, or > 10% band forms







Comments
Post a Comment