A CASE OF CKD ON MHD
MEDICINE CASE DISCUSSION
This is an E-log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence-based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed .
I have been given this case, in an attempt to solve and understand the topic of "Patient's clinical data analysis”. This has helped me develop my competency in reading and comprehending clinical data including history taking, clinical findings and investigations. The goal is to come up with a diagnosis and treatment plan.
75 year old male patient presented with CKD ON MHD
Abdominal distension since 20 days.
Swelling of B/L lower limbs since 20 days.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 20 days back when he developed abdominal distension which was insidious in onset and gradually progressive .It was associated with swelling of lower limbs upto knee joint on both sides.
Complaints of shortness of breath which was aggravated in supine position and relieved on sitting up(NYHA grade 4)
He also complaints of decreased frequency of urination since 20 days.
No c/o palpitations, cough, chest pain, syncopal attacks, PND.
No c/o abdominal pain, pruritis, hematuria, frothy urine.
The complaints relieved with treatment.
Since 4 days patient has been having vomiting (3 episodes /alternate day)with food as content.
He also has 5-7 episodes of loose stools daily which relieved with medication
Pruritis since 2 days
PAST HISTORY:
No similar complaints in the past
Not a k/c/o DM, HTN, asthma, thyroid disorder , epilepsy, CAD,CVA.
SYSTEMIC EXAMINATION:
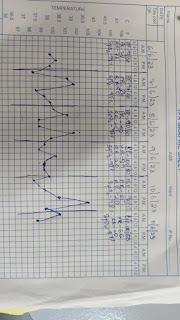
1/5/23:
3/5/23:
2D ECHO: (3/5/23)

.jpeg)

.jpeg)


.jpeg)






.jpeg)




Comments
Post a Comment