MEDICINE BLENDED ASSIGNMENT (MAY 2021) BY ROLL NUMBER 104
MEDICINE BLENDED ASSIGNMENT (MAY
2021)
I have been given the following cases
to solve in an attempt to understand the topic of 'Patient clinical
data analysis' to develop my competency in reading and comprehending clinical
data including history, clinical findings, investigations and diagnosis and
come up with a treatment plan.

This is the link of the questions asked regarding the cases:
http://medicinedepartment.blogspot.com/2021/05/online-blended-bimonthly-assignment.html?m=1
Below are my answers to the Medicine Assignment based on my comprehension of the cases.
PULMONOLOGY
CASE 1:
https://
i. What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
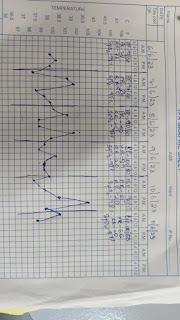
SYMPTOM TIMELINE:
ANATOMICAL LOCATION- LUNGS (bronchi and bronchioles) – lesions here led to increased pulmonary blood pressure thus causing Right Heart Failure.PRIMARY ETIOLOGY-This can be a case of allergic SOB as it occurs every year around the same time ,it could be due to allergy to paddy dust which is the patient’s area of work. The aggravating factor of this SOB could be use of CHULA as a method of cooking since many years.
ii. What is mechanism of action, indication and efficacy over placebo of each of the pharmacological and non-pharmacological interventions used for this patient?
Pharmacological interventions:
- Inj.augumentin-it’s a betalactum antimicrobial drug which inhibits the formation of peptidoglycan layer. It’s used to treat a number of bacterial infections.
- Tab.Azithromycin- It stops bacterial protein synthesis by inhibiting the transpeptidation/translocation step of protein synthesis and by inhibiting the assembly of the 50S ribosomal subunit .
- Inj.Lasix- it is a loop diuretic which acts by inhibiting the luminal Na-K-Cl cotransporter in the thick ascending limb of the loop of Henle and then binds to the chloride transport channel, thus causing sodium, chloride, and potassium loss in urine.
- it’s used to reduce extra fluid in the body (edema)
caused by conditions such as heart failure, liver disease, and kidney disease.
This can lessen symptoms such as shortness of breath and swelling in your arms,
legs, and abdomen. This drug is also used to treat high blood pressure.
- Tab.Pantop -It is a very commonly used antacid. It acts by inhibiting the final step in gastric acid production
- Inj.Hydrocortisone-It reduces the inflammation of a particular area by reducing the leukocyte migration to the injured area
- NEB. with IPRAVENT, BUDECORT -both of them act as bronchodilator and anti-inflammatory which is indicated in SOB
- Tab. Pulmoclear-Its used to loosen the mucosal layer .It is indicated in SOB.
- Inj.HAI-It is a fast-acting insulin which is given in diabetes
- Inj.Thiamine-given to correct vitb12 deficiency
Non-pharmacological interventions:
- Head elevation : Increases end expiratory lung volume and improves oxygenation.
- O2 inhalation : To manage hypoxia and increase oxyHb in RBC
- BiPAP intermittent : To relieve overworked lung and chest wall muscles (provides custom air pressure for inhalation and exhalation)
- Chest physiotherapy: To improve Respiratory efficiency and lung capacities by strengthening of chest wall muscles
- Vitals charting : For a constant check on patient
- Urine Input/output charting (I/O) - used to assess water/fluid dynamics in the body, depending upon fluid intake, urine volume and output over 24 hours.
Environmental pollutants can be a cause of her acute exacerbation’s other reason could be use of drugs for the treatment of TB which might have led to the exacerbation of her symptoms.
iv. Could the ATT have affected her symptoms? If so, how?
YES! The ATT has affected her symptoms as we know she was a known case of TB. The drugs used in the 1st line treatment of Tb such as isoniazid and rifampicin are known to be nephrotoxic in nature. This might have caused damage to the kidney which may have in turn lead to cardiorenal syndrome and effected the lungs .
v. What could be the causes for her electrolyte imbalance?
Following could be the possible causes of her electrolyte imbalance:
- Hypochloraemia-compressed respiratory acidosis
- Hyponatremia-right heart failure, respiratory acidosis, hypoxia.
NEUROLOGY
CASE 2A:
https://143vibhahegde.
i. What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
SYMPTOM TIMELINE:
ANATOMICAL LOCALIZATION :
Hippocampus.
PRIMARY ETIOLOGY : Vitamin B1 stores in body exhausted – biochemical lesions formed in the brain – thus the symptoms.
ii. What is mechanism of action, indication and efficacy over placebo of each of the pharmacological and non-pharmacological interventions used for this patient?
Kindling
: refers to the phenomenon of
increasingly severe withdrawal symptoms, including an increased risk of
seizures, that occurs as a result of repeated withdrawal from alcohol or other
sedative–hypnotics with related modes of action.
This
is what has happened with the patient which has lead to the neurological
symptoms this time-due to alcohol withdrawal.
Alcohol abuse with repeated withdrawal episodes lead to altered brain functions such as:
- Imbalance of inhibitory/excitatory neurotransmitters
- Neuroendocrine dysregulation
- Increased seizure susceptibility
- Increased anxiety
- Increased neurotoxicity
- Altered perceptions
All this ultimately lead to drinking relapse.
iv. What is the reason for giving thiamine in this patient?
Excessive
alcohol intake over prolonged periods cause deficiency of Vitamin B1(Thiamine)
in the body.
It
is needed for conduction of nerve signals – deficiency of the same leads to confusion and ataxia – both are
seen in this patient.
This is the reason why we have to give thiamine to the patient.
v. What is the probable reason for kidney injury in this patient?
The patients urea and creatinine levels
are high which is the cause of renal injury.
Diabetes can be a cause of kidney injury
or damage in this patient. Other cause can be dehydration due to excessive consumption
of alcohol.
vi. What is the probable cause for the normocytic anemia?
This is also known as anemia of chronic
disease.
The causes of the following can be:
- Chronic alcoholism
- Bleeding from the ulcer
- Kidney disease which can cause decreased production of erythropoietin.
vii. Could chronic alcoholism have aggravated the foot ulcer formation? If yes, how and why?
Chronic alcoholism can be a cause of
peripheral neuropathy which can cause diabetic neuropathy.
CASE 2B:
https://kausalyavarma.
i. What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary aetiology of the patient's problem?
SYMPTOM TIMELINE:
ANATOMICAL LOCALIZATION: right inferior cerebellar hemisphere
PRIMARY ETIOLOGY:
The main cause of the disease can be
high levels of cholesterol which has lead to embolization which had lead to the formation
of infract and hence the symptoms of ataxia.
ii. What is mechanism of action, indication and efficacy over placebo of each of the pharmacological and non-pharmacological interventions used for this patient?
iii. Did the patient’s history of denovo HTN contribute to his current condition?
Yes ,hypertension can be a cause of cerebellar
infraction also known as stoke.
The incidence of stroke increased progressively with degree of hypertension. The age- and sex-standardized incidences of cerebral infarction in subjects with hypertension grade 3 (≥180/110 mm Hg) and normal blood pressure (<140/90 mm Hg) were 6.8 and 1.7 per 1000 person-years.
iv. Does the patient’s history of alcoholism make him more susceptible to ischemic or hemorrhagic type of stroke?
Alcohol consumption can be a leading
cause of hemorrhagic stroke as the liver gets damaged due to excessive drinking
which can lead to stoke.
CASE 2C:
http://bejugamomnivasguptha.
i. What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary aetiology of the patient's problem?
SYMPTOM TIMELINE:
PRIMARY AETIOLOGY:
- Age > 40 years
- Female who has likely attained menopause may have Osteoporosis
- Degenerative Disc Disease
ii. What are the reasons for recurrence of hypokalaemia in her? Important risk factors for her hypokalaemia?
Hypokalemic periodic paralysis – a genetic disorder.
- Diuretics
- Inadequate intake: anorexia, dementia, starvation, total parental nutrition
- psuedohypokalemia
iii. What are the changes seen in ECG in case of hypokalaemia and associated symptoms?
Flattening and inversion of t-wave. QT interval prolongation and St depression in severe cases.
Associated symptoms: weakness, fatigue, muscle cramps, worsening of diabetes, palpitations
https://rishikoundinya.
i. Is there any relationship between occurrence of seizure to brain stroke? If yes what is the mechanism behind it?
A stroke occurs when the blood supply to part of your brain is interrupted or reduced, preventing brain tissue from getting oxygen and nutrients. Brain cells begin to die in minutes. A stroke is a medical emergency, and prompt treatment is crucial.
A seizure is a burst of uncontrolled electrical activity between brain cells (also called neurons or nerve cells) that causes temporary abnormalities in muscle tone or movements (stiffness, twitching or limpness), behaviors, sensations or states of awareness.
YES! There is a relation between seizure and brain stroke. A stroke causes your brain to become injured. The injury to your brain results in the formation of scar tissue, which affects the electrical activity in your brain. Disrupting the electrical activity can cause you to have a seizure.
ii. In the previous episodes of seizures, patient didn't lose his consciousness but in the recent episode he lost his consciousness what might be the reason?
Normally the “consciousness system”—a specialized set of cortical-subcortical structures—maintains alertness, attention and awareness. Diverse seizure types including absence, generalized tonic-clonic and complex partial seizures converge on the same set of anatomical structures through different mechanisms to disrupt consciousness.
CASE 2E:
https://nikhilasampathkumar.
i. What could have been the reason for this patient to develop ataxia in the past 1 year?
The possible cause of ataxia in this patient could be head injury caused due to multiple falls which has lead to intracranial hemorrhage causing pressure on brain areas and ataxia.
ii. What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses ?
In the new study, drinking alcohol causes liver damage - leading to decreased clumping of clotting cells in the blood. The impaired platelet function, together with the reduced platelet count, may contribute to the bleeding diathesis associated with chronic alcoholism.
Generally After minor head injuries the hemorrhage gets cured on itself if present.
But in this case as we know that the patient is a chronic alcoholic which might have stopped the process of healing or may have lead to increase in the size of hemorrhage. .
CASE 2F:
i. Does the patient's history of road traffic accident have any role in his present condition?
Yes! Occasionally strokes will occur following a neck, back or head injury sustained in an accident or because of medical negligence.
One of the case could be :Whiplash is usually a minor injury but sometimes it can have devastating effects. In serious cases, it can lead to severe long-term health problems. Whiplash injuries have the potential to cause damage to the main artery (the carotid artery) which supplies blood to the brain, resulting in a stroke. Initially a minor injury – such as whiplash – may not appear to have a life-changing impact, but sadly it can develop into a stroke several weeks later.
ii. What are warning signs of CVA?
The five warning
signs of stroke are:
- Sudden
onset of weakness or numbness on one side of the body.
- Sudden
speech difficulty or confusion.
- Sudden
difficulty seeing in one or both eyes.
- Sudden
onset of dizziness, trouble walking or loss of balance.
- Sudden, severe headache with no known cause.
- Aspirin(antiplatelet drug)-ecosprin- Aspirin irreversibly inhibits cyclooxygenase, which prevents the conversion of arachidonic acid to thromboxane A2 (TXA2). Thromboxane A2 is a vasoconstrictor and stimulator of platelet aggregation. Platelets are inhibited for their full life cycle (5–7 days) after exposure to aspirin. Aspirin also inhibits prostacyclin activity and this inhibits platelet aggregation.
- Mannitol-The role of mannitol therapy in acute stroke is controversial. Because of its osmotic effect, mannitol is assumed to decrease cerebral edema. Mannitol might improve cerebral perfusion by decreasing viscosity, and as a free-radical scavenger, it might act as a neuroprotectant.
What is SNSS score and how is it important?
Atorvastatin belongs to a group of medicines called statins. It's used to lower cholesterol if you've been diagnosed with high blood cholesterol. It's also taken to prevent heart disease, including heart attacks and strokes. Atorvastatin is in a class of medications called HMG-CoA reductase inhibitors (statins). It works by slowing the production of cholesterol in the body to decrease the amount of cholesterol that may build up on the walls of the arteries and block blood flow to the heart, brain, and other parts of the body.
QUESTIONS:
a. What are the other drugs that can be given in a stoke?
b. What is the other drug we can use instead of mannitol?
iv. Does alcohol have any role in his attack?
Many risk factors contribute to stroke such as:
- Hypertension
- Diabetes
- Obesity
- Liver disease
- Cardiac disorders such as atrial fibrillation
The important thing to note is that all of these factors are linked to alcohol use. Specifically, research has also shown that people who are middle-aged and drink have a 1/3 higher risk for stroke and people classified as heavy drinkers have a higher chance of suffering a stroke at a younger age. In one particular study, it was shown as having more than two drinks a day. People who had more than two drinks a day, as compared to very light drinkers who had half a drink a day, had a 34 percent higher risk of stroke, and their stroke was five years earlier on average. This shows that alcohol is a very significant risk factor for stroke.
v. Does his lipid profile have any role for his attack??
YES! According to the study below there might be a relation with lipid profile in the patient
Few studies have compared serum HDL-C against serum LDL-C to determine relative contributions to stroke risk. In one study of the very old (aged ≥85 years) low serum HDL-C was associated with an increased risk of stroke, cardiovascular disease, and mortality whereas LDL-C and total cholesterol had no association. On the other side of the age spectrum, a study of young stroke patients demonstrated that low HDL-C was the only serum lipid index associated with an increased risk of stroke. Low HDL-C was associated with a significant increase in carotid plaque volume by ultrasound. The association of low HDL with increased plaque volume was strengthened when patients on cholesterol-lowering agents were excluded and may indicate an independent effect of HDL-C.
https://www.ahajournals.org/doi/10.1161/01.str.0000258347.19449.0f#:~:text=Few%20studies%20have%20compared%20serum,total%20cholesterol%20had%20no%20association
CASE 2G:
https://amishajaiswal03eloggm.
i. What is myelopathy hand ?
MYELOPATHY HAND: Cervical myelopathy is a common degenerative condition caused by
compression on the spinal cord that is characterized by clumsiness in hands and
gait imbalance
There is loss of power of adduction and extension of the ulnar two or
three fingers and an inability to grip and release rapidly with these fingers.
These changes have been termed "myelopathy hand" and appear to
be due to pyramidal tract involvement.
Clinical signs in myelopathy-together called as myelopathy hand
- Finger escape sign
- Impaired finger motion
- Slow grip and release
- Paradoxical wrist motion etc.
Aetiology-
- Degenerative cervical spondylosis
- Congenital stenosis
- Epidural abscess
- Tumour
Symptoms-
- Clumsiness
- Finger escape sign
- Grip and release test
- Intrinsic wasting
Demonstration of myelopathy hand: https://youtu.be/sdUr3CMebBw
ii. What is finger escape ?
Finger escape sign-
Also known as the wartenbergs sign in cervical
myelopathy.
Wartenberg's
sign is a neurological sign consisting of involuntary abduction of the fifth
(little) finger, caused by unopposed action of the extensor digiti minima.
... This finding of weak finger adduction in cervical
myelopathy is also called the "finger escape sign".
A
method of surgical correction is described for Wartenberg's sign,
or persistent abduction of the little finger, using a slip of the extensor digitorum
communis of the ring finger. The transferred component can be either the
central slip, or the ulnar slip extended by the connexus intertendineus to the
little finger.
For
clinical demonstration of wartenberg’s sign:
iii. What is Hoffman’s reflex?
Hoffman’s
sign/reflex:
Hoffman's sign or reflex is a test that doctors use
to examine the reflexes of the upper extremities. This test is
a quick, equipment-free way to test for the possible existence of spinal cord
compression from a lesion on the spinal cord or another underlying nerve
condition.
Procedure:
The
Hoffmann's reflex test itself involves loosely holding the middle finger and
flicking the fingernail downward, allowing the middle finger to flick upward reflexively.
Interpretation:
Positive test- A positive response is seen when there is flexion and adduction of the thumb on the same hand. A positive Hoffmann’s reflex and finger jerks suggest hypertonia, but can occur in healthy individuals, and are not useful signs in isolation
Negative test-seen when there is acute inflammatory demyelinating polyneuropathy (Guillain–Barré syndrome). This loss of H reflexes occurs early and may be an isolated finding in patients studied within several days after onset of illness.
CASE 2H:
https://neerajareddysingur.
i. What can be the cause of her condition ?
The causes of seizures in this patient can be:
Cortical vein thrombosis with hemorrhagic venous infarction in right posterior temporal lobe .
OTHER CAUSES COULD BE:
- Electrolyte imbalance(hypomagnesemia)
- Iron deficiency anaemia(mainly in endemic area of malaria)
- hypoglycaemia
Cerebral venous sinus thrombosis (CVST) occurs when a blood clot forms in the brain’s venous sinuses. This prevents blood from draining out of the brain. As a result, blood cells may break and leak blood into the brain tissues, forming a haemorrhage.
Risk factors for
children and infants include:
- Problems
with the way their blood forms clots
- Sickle
cell anaemia
- Chronic
haemolytic anaemia
- Beta-thalassemia
major
- Heart
disease — either congenital (you're born with it) or acquired (you develop
it)
- Iron
deficiency
- Certain
infections
- Dehydration
- Head
injury
- For new-borns,
a mother who had certain infections or a history of infertility
Risk factors for
adults include:
- Pregnancy
and the first few weeks after delivery
- Problems
with blood clotting; for example, antiphospholipid syndrome, protein C and
S deficiency, antithrombin III deficiency, lupus anticoagulant, or factor
V Leiden mutation
- Cancer
- Collagen
vascular diseases like lupus, Wegener’s granulomatosis, and Behcet
syndrome
- Obesity
- Low
blood pressure in the brain (intracranial hypotension)
- Inflammatory
bowel disease like Crohn’s disease or ulcerative colitis
iii. There was seizure free period in between but again sudden episode of GTCS why? Resolved spontaneously why?
iv. What drug was used in suspicion of cortical venous sinus thrombosis?
Acitrom tablet is an oral anticoagulant medicine that is used for the treatment and prevention of the formation of abnormal blood clots (thrombus) in blood vessels and disease associated with it affect. Acitrom works by inhibiting the action of an enzyme responsible for the formation of blood clots
CARDIOLOGY
CASE 3A:
https://muskaangoyal.blogspot.
i. What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
Preserved ejection fraction (HFpEF) – also referred to as diastolic heart failure. The heart muscle contracts normally but the ventricles do not relax as they should during ventricular filling (or when the ventricles relax).
Reduced ejection fraction (HFrEF) – also referred to as systolic heart failure. The heart muscle does not contract effectively, and therefore less oxygen-rich blood is pumped out to the body.
ii. Why haven't we done pericardiocentesis in this patient?
The indications of pericardiocentesis are:
- Cardiac tamponade-the patient does not have it
- Chronic pericardial effusion-the patient has moderate pericardial effusion
- Highly suspected tuberculosis, purulent or neoplastic aetiology-the patient does not have tuberculosis
Risk factors for heart failure in the patient
- Hypertension
- Diabetes
- Smoking
- Alcoholic
iv. What
could be the cause for hypotension in this patient?
The cause of hypotension in this patient can be not enough filling of the heart with blood due to pressure on the walls of the heart.
CASE 3B:
https://muskaangoyal.blogspot.
1.What are the possible causes for heart failure in this patient?
Causes of heart failure in the patient are:
- Myocarditis. Myocarditis is an inflammation of the heart muscle. It's most commonly caused by a virus, including COVID-19, and can lead to left-sided heart failure.
- Hypertension
- Diabetes
- Alcohol use. Drinking too much alcohol can weaken heart muscle and lead to heart failure.
- Obesity
2.what is the reason for anaemia in this case?
The most common cause of anaemia in this patient can be chronic kidney disease
Other causes can be old age ,alcohol use causing malnutrition and anaemia
3.What is the reason for blebs and non-healing ulcer in the legs of this patient?
Diabetes can be a cause of bleps and non-healing ulcer
4. What sequence of stages of diabetes has been noted in this patient?CASE 3C:
https://preityarlagadda.
i. What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary aetiology of the patient's problem?
SYMPTOM TIMELINE:
ANATOMICAL LOCALISATION : Initially Kidney then Heart.PRIMARY AETIOLOGY : Hypertension which resulted in chronic kidney disease.
ii. What is mechanism of action, indication and efficacy over placebo of each of the pharmacological and non-pharmacological interventions used for this patient?
- TAB. Dytor 10mg PO/OD
- TAB. Acitrom 2mg PO/OD
An oral anticoagulant medicine that is used for the treatment and prevention of the formation of abnormal blood clots (thrombus) in blood vessels and disease associated with it affect. Acitrom works by inhibiting the action of an enzyme responsible for the formation of blood clots
- TAB. Cardivas 3.125mg PO/BD
An alpha and beta blocker. It works by slowing down the heart rate and relaxing blood vessels which makes the heart more efficient at pumping blood around the body.
- INJ. HAI S/C 6U-6U-4U
It is a short-acting insulin. It works by helping blood sugar (glucose) get into cells so your body can use it for energy. This medication is usually used in combination with a medium- or long-acting insulin product. This medication may also be used alone or with other oral diabetes drugs
- TAB. Digoxin 0.25mg OD 5/7 except Saturday and Sunday
Helps an injured or weakened heart pump more efficiently. It strengthens the force of the heart muscle's contractions, helps restore a normal, steady heart rhythm, and improves blood circulation
- Hypoglycaemia symptoms explained
- Watch for any bleeding manifestations like Petechiae, Bleeding gums.
- PT, INR, APTT after 15 days and Review sos. -AS WHEN a person is on anticoagulant therapy to make sure that drug is producing desired out come
iv. What are the risk factors for atherosclerosis in this patient?
Effect of hypertension:
They can also impair blood vessels' ability to relax and may stimulate the growth of smooth muscle cells inside arteries. All these changes can contribute to the artery-clogging process known as atherosclerosis. hypertension appears to increase the susceptibility of the small and large arteries to atherosclerosis.
v. Why was the patient asked to get those APTT, INR tests for review?
APTT and INR are ordered on a regular basis when a person is taking the anticoagulant drug warfarin to make sure that the drug is producing the desired effect.
Here, an INR of 3-4.5 is recommended. Warfarin should be started in conjunction with heparin or low molecular weight heparin when the diagnosis of venous thromboembolism is confirmed, although local protocols may vary in their starting doses and titration schedule.
CASE 3D:
i. What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary aetiology of the patient's problem?
SYMPTOM TIMELINE;
ANATOMICAL LOCALIZATION: heart
PRIMARY ETIOLOGY:
Acute coronary syndrome usually results from the buildup of fatty deposits (plaques) in and on the walls of coronary arteries, the blood vessels delivering oxygen and nutrients to heart muscles.
When a plaque deposit ruptures or splits, a blood clot forms. This clot blocks the flow of blood to heart muscles.
The risk factors for this patient could be diabetes and hypertension.
ii. What is mechanism of action, indication and efficacy over placebo of each of the pharmacological and non-pharmacological interventions used for this patient?
TAB MET XL 25 MG/STAT.-works by relaxing the blood vessels, thus slowing down the heart rate. By doing this, it reduces the workload on the heart of pumping the blood effectively. It is a beta blocker which is indicated in hypertension, angina and arrtymias.
iii. What are the indications and contraindications for PCI?
INDICATIONS
- Acute ST-elevation myocardial infarction (STEMI)
- Non–ST-elevation acute coronary syndrome (NSTE-ACS)
- Unstable angina.
- Stable angina.
- Anginal equivalent (e.g., dyspnea, arrhythmia, or dizziness or syncope)
- High risk stress test findings.
- Intolerance for oral antiplatelets long-term.
- Absence of cardiac surgery backup.
- Hypercoagulable state.
- High-grade chronic kidney disease.
- Chronic total occlusion of SVG.
- An artery with a diameter of <1.5 mm.
PCI is generally a safe procedure , it might cause serious certain complications like
- Bleeding
- Blood vessel damage
- Allergic reaction to the contrast dye used
- Arrhythmias
- Need for emergency coronary artery bypass grafting
CASE 3E:
https://bhavaniv.blogspot.com/
i. What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary aetiology of the patient's problem?
SYMPTOM TIMELINE:
ANATOMICAL LOCALIZATION: Heart
PRIMARY ETIOLOGY: patient is a known case of diabetes and hypertension which are risk factors for the development of cardiovascular disorders.
ii. What is mechanism of action, indication and efficacy over placebo of each of the pharmacological and non-pharmacological interventions used for this patient?
iii. Did the secondary PTCA do any good to the patient or was it unnecessary?
PCI performed from 3 to 28 days after MI does not decrease the incidence of death, reinfarction or New York Heart Association (NYHA) class IV heart failure but it is associated with higher rates of both procedure-related and true ST elevation reinfarction.
CASE 3F:
https://kattekolasathwik.
i. How did the patient get relieved from his shortness of breath after i.v fluids administration by rural medical practitioner?
As the patient was under hypovolemic shock, there was a fall in his fluid levels. To prevent any complications, IV fluids were administered and after fluid restoration, there was relieve from dyspnea.
ii. What is the rationale of using torsemide in this patient?
Torsemide is a high efficacy diuretic which works by blocking Na-K-2Cl cotransporter, causing their excretion and hence creating diuresis
It was used in the patient as he was suffering from pulmonary edema and it caused diuresis helping reduce the fluid volume
iii. Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
Ceftriaxone is used to treat a wide variety of bacterial infections.It was given for the treatment of UTI .
It was mainly for the prophylactic use as the patient has CARDIORENAL SYNDROME.
GASTROENTROLOGY AND PULMOLOGY
CASE 4A:
https://63konakanchihyndavi.
i. What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary aetiology of the patient's problem?
SYMPTOM TIMELINE:
ANATOMICAL LOCALIZATION-- Sub-hepatic region
- Body of the pancreas
- Left basilar segment of lung
ii. What is the efficacy of drugs used along with other non-pharmacological treatment modalities and how would you approach this patient as a treating physician?
Treatment modalities:
- meropenem-preventing septic complications.
- metronidazole-successful in the treatment of acute pancreatitis.it reduces drug resistance when used in combination therapy.
- amikacin-helps to kill the gram negative bacteria hence used widely in abdominal sepsis.
- octreotide.
- non pharmacological-fasting, treating dehydration,pain medication and a low fat diet
CASE 4B:
https://nehae-logs.blogspot.
i. What is causing the patient's dyspnea? How is it related to pancreatitis?
DYSPNEA is caused because of pleural effusion in this patient.
Pancreatitis in its severe form is complicated by multiple organ system dysfunction, most importantly by pulmonary complications which include hypoxia, acute respiratory distress syndrome, atelectasis, and pleural effusion.
with severe pancreatitis there are a lot of inflammatory chemicals that are secreted into the blood stream. These chemicals create inflammation throughout the body, including the lungs. As a result, a person may experience an inflammatory type of reaction in the lungs called ARDS.
Reference link:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5793936/
ii. Name possible reasons why the patient has developed a state of hyperglycaemia.
Hyperglycemia: increased blood sugar levels (>140mg/dl).
From the given data of the patient there can be three reasons for the above
- Age of the patient-52years very common to develop Type-2 DM
a .impaired beta-cell functions b .insulin resistance
- He is known to be consuming alcohol from past 4 years.
- We can say that the pancreas of the patient is affected. As we know that pancreas are the organ in our body which help in formation of insulin
iii. What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
- LFT are increased due to hepatocyte injury.
- If the liver is damaged or not functioning properly, ALT can be released into the blood. This causes ALT levels to increase. A higher than normal result on this test can be a sign of liver damage
- Elevated alanine transaminase (ALT) and aspartate transaminase (AST), usually one to four times the upper limits of normal in alcoholic fatty liver.
- Specific marker for Alcoholic Fatty Liver disease - GGT (Gamma-Glutamyl Transferase)
iv. What is the line of treatment in this patient?
Treatment:
• IVF: 125 mL/hr
• Inj PAN 40mg i.v OD
• Inj ZOFER 4mg i.v sos
• Inj Tramadol 1 amp in 100 mL NS, i.v sos
• Tab Dolo 650mg sos
• GRBS charting 6th hourly
• BP charting 8th hourly
CASE 4C:
https://chennabhavana.
i. What is the most probable diagnosis in this patient?
The most probable diagnosis of the case is LIVER ABSCESS
ii. What was the cause of her death?
Septicemia causing multiorgan failure is the most probable cause of her death.
iii. Does her NSAID abuse have something to do with her condition? How?
NSAID-induced renal dysfunction has a wide spectrum of negative effects, including decreased glomerular perfusion, decreased glomerular filtration rate, and acute renal failure.
NEPHROLOGY AND UROLOGY
CASE 5A:
https://kavyasamudrala.
i. What could be the reason for his SOB?
Post TURP with ATN
Acute tubular necrosis leads to retention of fluid in lungs
Edema in lungs lead to shortness of breath
ii. Why does he have intermittent episodes of drowsiness?
Patient shows elevated levels of urea and creatinine in RFT due to kidney injury
This increased creatinine is the cause of drowsiness and altered mental state .Uremic Encephalopathy is the likely cause for the patient's drowsiness.
iii. Why did he complaint of fleshy mass like passage in his urine?
During Transurethral resection of the prostate ( TURP ) surgery ,we do electrocautery to minimise bleeding .This blood may clot and form scab ,Clot retention is one of the common complications of TURP
This scab is passed from urethra following surgery , which is perceived by patient as passage of mass
iv. What are the complications of TURP that he may have had?
Major:
- Clot retention
- Failure to void
- Uncontrolled acute hematuria
- UTI
- Chronic hematuria
- Bladder perforation
- Sepsis
- DIC
CASE 5B:
https://drsaranyaroshni.
1.Why is the child excessively hyperactive without much of
social etiquettes?
The reason for his hyperactivity could be ADHD (Attention deficit hyperactivity disorder)
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder characterized by inattention, or excessive activity and impulsivity.
2. Why doesn't the child have the excessive urge of urination at night time?
The child doesn’t show symptoms of nocturnal enuresis
This points towards psychosomatic origin of disease i e . anxiety ,stress etc.
3. How would you want to manage the patient to relieve him of his symptoms?
1) Further investigations to rule out any organic cause . This includes :
Proper USG
Complete blood count
Blood and urine sugars
2) Diagnosis of any anxiety disorder if present
3) In the absence of organic cause , treatment would be BEHAVIOURAL THERAPY
4) Ditropan – to decrease urgency and frequency of urination
5) Assurance to mother and child
INFECTIOUS DISEASE (HIV,MYCOBACTERIA,GASTROENTEROLOGY,PULMONOLOGY)
CASE 6A:
https://vyshnavikonakalla.
i. Which clinical history and physical findings are characteristic of tracheo oesophageal fistula?
History:
- C/O difficulty in swallowing i. e . Dysphagia
- C/O cough on food intake
- H/O retroviral disease
- Laryngeal crepitus
- Endoscopy showing large opening with proliferative growth in mid esophagus
- CECT : Fistulous communication between left main bronchus and mid thoracic esophagus
- Barium swallow showing abnormal contrast due to communication between esophagus and bronchial tree
ii. What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
The chances of development of immune reconstitution inflammatory syndrome in this patient is high .
The following are the risk factors present in this patient :
- Fever since 2 months
- Diagnosis of TB after initiation of ART
- Lymph node enlargement in mediastinum
- CRP + ve
INFECTIOUS DISEASE AND HEPATOLOGY
CASE 7A:
https://kavyasamudrala.
i. Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors present in it? What could be the cause in this patient?
Cause of liver abscess in this patient is consumption of locally brewed toddy
Yes , locally made alcohol acted as factor for liver abscess in this patient Poor economic conditions lack of sanitation and malnutrition could also play a role as predisposing factors.
ii. What is the etiopathogenesis of liver abscess in a chronic alcoholic patient? ( Since 30 years - 1 bottle per day)
Liver abscess can be pyogenic ,amoebic or hydatid
Infections are acquired from blood stream ( portal and systemic circulation)
The most common pathophysiology is bowel content leakage and peritonitis . Bacteria travel via portal blood vessels into liver .
In this case , Alcohol consumption specially locally prepared alcohol plays major role in liver abscess ( pyogenic and amoebic )
Alcohol acts as predisposing factor
Factors responsible for association between alcohol and liver abscess are as follows:
Poor nutritional status due to alcohol consumption
Presence of infective organisms in the locally prepared alcohol .
Immunity of the patient
Damage to liver done by alcohol
iii. Is liver abscess more common in right lobe?
Yes ,liver abscess is more common in right lobe compared to left lobe
Single lesions are more common in right lobe
This is attributed to comparatively more blood supply via superior mesenteric vein on right side
iv. What are the indications for ultrasound guided aspiration of liver abscess ?
- If the abscess is large ( 5cm or more) because it has more chances to rupture.
- If the abscess is present in left lobe as it may increase the chance of peritoneal leak and pericardial leak.
- If the abscess is not responding to the drugs for 7 or more days.
CASE 7B:
https://63konakanchihyndavi.
i. Cause of liver abscess in this patient?
Most common cause of a liver abscess is amoebic infection are caused by Entamoeba histolytica. The pyogenic abscesses can also be a potential cause by bacteria that include E.coli, Klebsiella, Streptococcus, Staphylococcus, and anaerobes.If the cause is infectious, the majority of liver abscesses can be classified into bacterial (including amebic) and parasitic sources (including hydatiform cyst).
ii. How do you approach this patient?
Treatment of liver abscess :
- Empirical antibiotics : cover both bacterial and amoebic causes
- For bacterial cause : penicillin +cephalosporin is given ( zostum 1.5 gm i.v. BD injection)
- For amoebic cause : metronidazole ( Metrogyl 500mg i.v. TID injection
- Percutaneous drainage of abscess is not done in this patient because of the response to antibiotic therapy and associated complications of drainage
- Ultracet to relieve pain
- Dolo 650 mg for fever
iii. Why do we treat here ; both amoebic and pyogenic liver abscess?
The liver abscess is of an unknown etiology. Hence empirical treatment for both the types of liver abscesses is being administered.
Metronidazole is for the amoebic type of abscess and Sulbactam and cefoperazone are broad spectrum antibiotics for the pyogenic liver abscess.
iv. Is there a way to confirm the definitive diagnosis in this patient?
The diagnosis can be done by the following:
- Detection of serum antibodies against Entamoeba
- Culture and sensitivity report of the aspirate
INFECTIOUS DISEASE
(MUCOR MYCOSIS ,OPHTHALMOLOGY,OTORHINOLARYNGOLOGY,NEUROLOGY)
CASE 8A:
http://manikaraovinay.
i. What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
SYMPTOM TIMELINE:
ANATOMICAL LOCALIZATION:- Eye
- Nasal & sinus mucosa
- Oral cavity
- Brain
PRIMARY ETIOLOGY:
Rhizopus : fungus
Mucormycosis (previously called zygomycosis) is a serious but rare fungal infection caused by a group of molds called mucormycetes. These molds live throughout the environment.
ii. What is the efficacy of drugs used along with other non-pharmacological treatment modalities and how would you approach this patient as a treating physician?Drugs that can be used to treat mucormycosis are:
- Amphotericin – B
- Liposomal
- Deoxycholate
- Posaconazole
- Liposomal AmpB > Deoxycholate AmpB > Posaconazole
- Deoxycholate AmpB is cheaper compared to Liposomal AmpB
Approach to patient:
- Stabilise the patient
- Treat the diabetic ketoacidosis
- Treatment with antifungal preferably Liposomal AmpB
iii. What are the postulated reasons for a sudden apparent rise in the incidence of Mucor mycosis in India at this point of time?
The reason for recent increase in the cases of mucormycosis is immunocompromised state following recovery from COV.
INFECTIOUS DISEASE(COVID 19)
http://medicinedepartment.
Please find my master sheet below.
https://docs.google.com/spreadsheets/d/1zqyoxOzMNVlXV0iTHxj8cJhQkvagFZMSDCYJXfcgedA/edit?usp=sharing
MEDICAL EDUCATION
I have learned a lot from this way to eloging the cases. I am grateful to Dr.rakesh biswas sir for giving us this opportunity even in these hard covid times.I would like to thank all the proffesors, postgraduates and interns who have helped us in the way .
elog of a patient done with the help of Dr.sai charan
https://pavitrabaldawa.blogspot.com/2021/05/a-case-of-cerebrovascular-accident.html





























































Comments
Post a Comment