MEDICINE CASE DISCUSSION
This is an E-log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence-based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed .
I have been given this case, in an attempt to solve and understand the topic of "Patient's clinical data analysis”. This has helped me develop my competency in reading and comprehending clinical data including history taking, clinical findings and investigations. The goal is to come up with a diagnosis and treatment plan.
HALL TICKET NO-1701006137
12TH JUNE 2022
FINAL PRACTICAL-SHORT CASE
CHIEF COMPLAINS:
A 35 year old male patient bartender by occupation and a resident of Khammam ,came to the medicine OPD with chief complains of
Breathlessness since 10 days
Palpatations since 7 days
Cough since 2 days
HISTORY OF PRESENTING ILLNESS:
The patient was apparently asymptomatic 1 month ago ,then he developed shortness of breath which was insidious in onset and gradually progressive since 10 days which progressed from no limitation in ordinary activity (grade 1) to slight limitation in physical activity(grade2)(according to NYHA GRADING )
The breathlessness aggravated on lying down and was relieved on rest and with medications
This worsened 7 days ago when he started developing shortness of breath at rest which was associated with palpations.
The palpations were sudden in onset and not associated with chest pain or sweating.
The patient had 3 episodes of paroxysmal nocturnal dyspnea the previous night, due to which he had to stay up all night.
He developed bilateral pedal edema below the knees 2 days ago which was insidious in onset and gradually progressive, no aggravating and relieving factors .
The patient also complained of cough since 2 days which was insidious in onset ,which was dry at first and the progressed to cough with sputum
It was in small amount ,mucopurulent in nature ,non foul smelling ,non blood stained.
No history of fever ,vomiting ,loose stools, decreased urine output.
History of alcohol binge 1 week prior to development of palpatations.
PAST HISTORY:
No history of similar complains in the past.
Not a known case of DM ,HTN ,Epilepsy, Asthma , thyroid disorder
No previous blood transfusions.
No known surgical history.
PERSONAL HISTORY :
The patient consumes a mixed diet
Appetite is normal
Bowel and Bladder movements are regular
Sleep is disturbed since 10 days
Addictions- Alcohol intake every day since the past 15 years about 180 ml per day
He has a continuous exposure to smoke .
FAMILY HISTORY:
No similar complains in the family.
GENERAL EXAMINATION:
Examined in a well lit room with proper consent
Patient is conscious, coherent and co-operative.
Moderately built and nourished.
Truncal obesity is present.
No pallor , icterus, cyanosis, clubbing, lymphadenopathy and edema.
Vitals:
Temperature- Afebrile
Respiratory rate - 18cpm
Pulse rate- 165bpm
Blood pressure- 110/80mmhg
SPO2-98%
GRBS-132mg/dl post prandil
SYSTEMIC EXAMINATION:
Cardiovascular system:
INSPECTION:
Shape of the chest and symmetry: Normal - bilaterally symmetrical
Breast abnormalities: Absent
Spine deformities: Absent
Apical impulse:Not visible
Pulsations - Absent
Dilated veins : Absent
PALPATION:
Inspectory findings are confirmed
Apex beat is felt in the 6 th intercoastal space , 2-3 cm from the mid clavicular line .
No parasternal heave felt.
No thrill.
PERCUSSION:
Dullness corresponding to Right Heart border is normal
Dullness corresponding to left heart border is shifted 2cm laterally
AUSCULATION:
S1 and S2 heard
No murmurs are heard.
Central nervous system:
Conscious and coherent , normal sensory and motor responses
Respiratory system:
Normal vesicular breath sounds and bilateral entry of air
Per abdomen:
Soft and tender . No organomegaly.
INVESTIGATIONS:
8th june 2022:
serum creatinine : 1.0 mg\dl
blood urea : 22mg\dl
serum electrolytes : Na+ - 138 mEq\L
K+ - 3.9
Cl- - 100
ABG:
Ph : 7.43
PCo2 : 26.8 mmHg
PO2 : 76.3 mmHg
HCo3: 17.6 mmol\L
St. HCo3 : 20.4 mmol\L
TCo2 : 35
O2 stat : 94.0
HEMOGRAM :
hemoglobin : 12.0 gm\dl
TLC : 14,000
PCV : 37.6
MCV : 70.9
MCH : 22.4
RDW-CV : 16.9
LIVER FUNTION TESTS :
total bilirubin : 2.32
direct bilirubin : 0.64
SGPT : 58
SGOT : 34
9th june 2022
Ph : 7.43
PCo2 : 26.8 mmHg
PO2 : 76.3 mmHg
HCo3: 17.6 mmol\L
St. HCo3 : 20.4 mmol\L
TCo2 : 35
O2 stat : 94.0
10 th june 2022
HEMOGRAM :
Hb : 11.3
TLC : 17,100
platelets : 3.43
serum creatinine : 1.1mg\dl
11th june 2022
HEMOGRAM :
Hb : 12.8
total count : 14,100
platelets : 3.93
RBC : 6.04 millions\cumm
XRAY:
ECG:
2D ECHO
PROVISIONAL DIAGNOSIS:
This is a case of atrial fibrillation and dilated cardiomyopathy.
TREATMENT:
Inj AMIODARONE 900mg in 32 ml normal saline @ 0.5mg\min
Inj AUGMENTIN 1.2gm\IV\BD
Tab AZITHROMYCIN 500mg PO\BD
Inj HYDRODRT 100mg IV\BD
Neb with DUOLIN @ 8th hourly
BUDSCORT @ 8th hourly
Inj LASIX 40mg\IV\BD
Inj THIAMINE 200mg in 50ml normal saline IV\TID
Tab CARDARONE 150mg
Tab clopitab 75mg RO OD
Tab ATROVAS 80MG
Fluid restriction <1.5L per day
Salt restriction <4gm per day
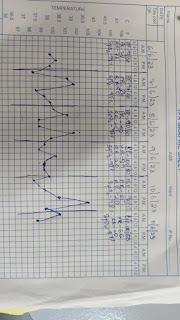
Strict temperature chart 4th hourly





.jpeg)
.jpeg)

.jpeg)
.jpeg)

.jpeg)

Comments
Post a Comment