MEDICINE CASE DISCUSSION
MEDICINE CASE DISCUSSION
This is an E-log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence-based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed .
I have been given this case, in an attempt to solve and understand the topic of "Patient's clinical data analysis”. This has helped me develop my competency in reading and comprehending clinical data including history taking, clinical findings and investigations. The goal is to come up with a diagnosis and treatment plan.
PAVITRA BALDAWA
ROLL NUMBER -104
3 RD FEBURARY 2022
CHIEF COMPLAINS:
35 year old male came to our hospital with chief complaints of upper abdomen pain since one week, fever since one week.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 1 week ago, then developed pain abdomen which was insidious in onset, gradually progressive. Pain in right hypochondrium and gastric region radiating towards back with no aggravating and relieving factors.
Fever is on and off since one week, high grade not associated with chills and rigor, cold, cough, body pains, nausea vomitings, loose stools and constipation.
No history of bleeding manifestations.
PAST HISTORY:
Not a k/c/o T2DM,HTN,asthma , epilepsy,TB
PERSONAL HISTORY:
Diet - mixed
Appetite - decreased since 1 week
Sleep- inadequate due to pain
Bowel movements- normal
Addictions- alcohol, regular, since 10 years
Smoking, 10 pack years
General physical examination
Pt is conscious, coherent, cooperative,
Icterus- present
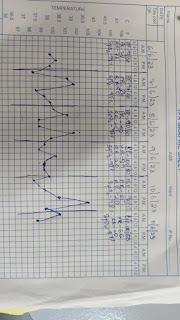
Vitals-
Temp- afebrile
Bp-110/70 mm hg
Pr- 86 bpm
Rr-20 cpm
Spo2- 98% on RA
Vitals on 2-2-22
Bp 100mmhg
Pulse 72
SpO2 - 98
Resp - 24 bpm
Systemic examination
RS- bae+, nvbs
Cvs-S1 S2 +
P/A -
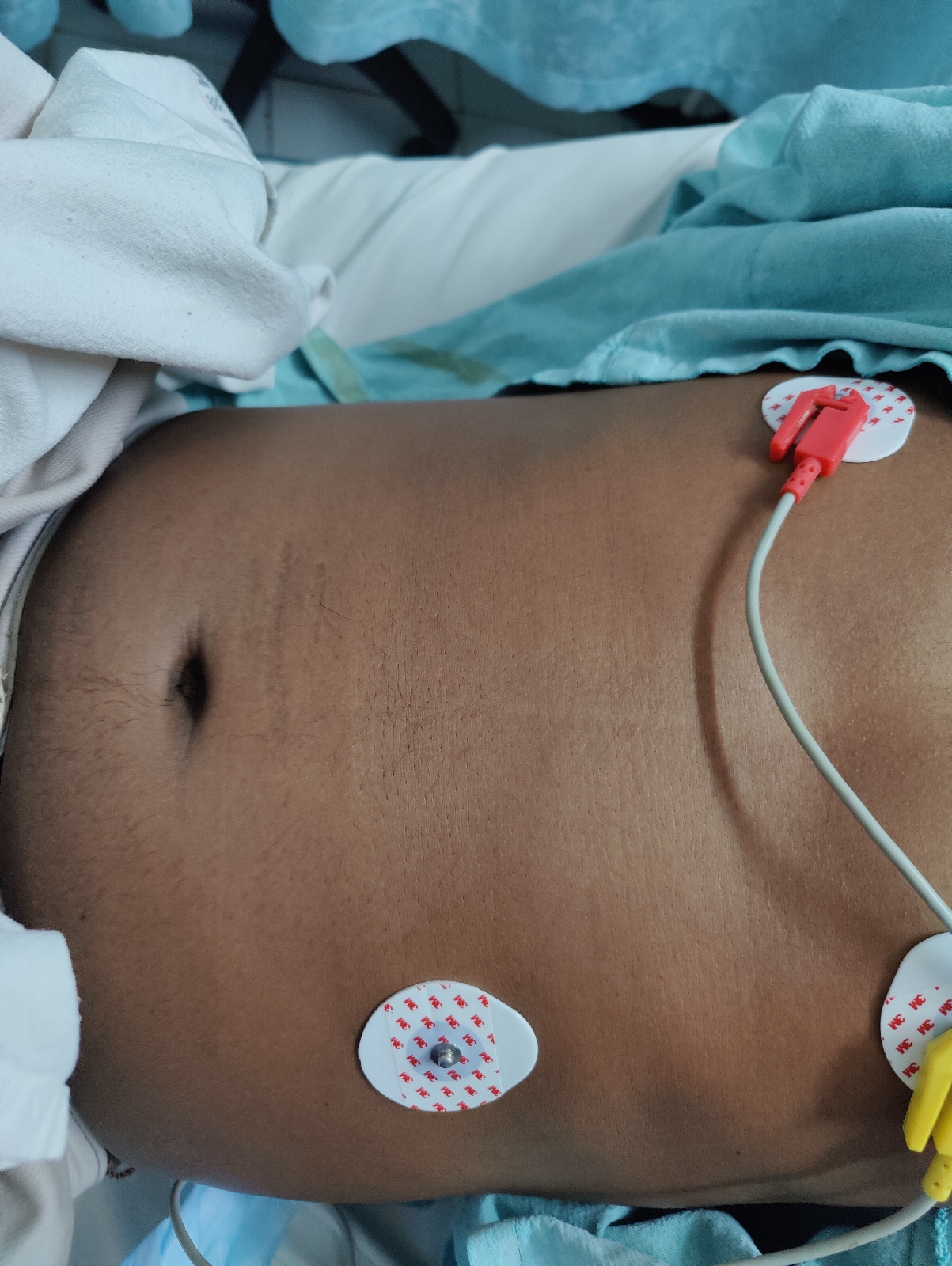
Inspection:
Shape - distended ,uniformly
Umbilicus - centrally positioned , inverted
Skin - stretched
No dilated veins
On superficial palpation:
tenderness + at right hypochondrium and epigastric region, umbilical and Rt lumbar
Auscultation:
Sluggish bowel sounds heard
Cns- nad
X-ray erect abdomen
Diagnosis
Liver abscess
Plan of treatment
1. Inj. Metrogyl 100 ml/IV/TID
2. Inj. Pantop 40 mg/IV/OD
3. Inj. Piptaz 4.5 gm/IV/TID
4. Inj. Tramadol 1amp in 100mg
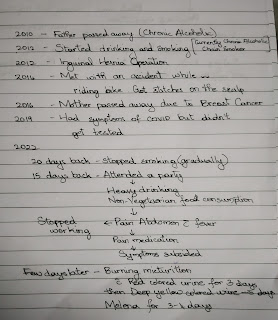
Time line
USG -shows 50% liquefaction
Day 2
S - pain abdomen subsides
One fever spike in morning
O - on examination
Patient is concious, cherent
Icterus- present
Vitals-
Temperature- 99.6
Pulse rate- 96
Blood pressure- 110/80
Respiratory rate- 22
Spo2- 96% at room air
Systemic examination-
Cardiovascular system- S1 and S2 heard, no murmurs
Respiratory system- bilateral air entry present, normal vesicular breath sounds
Central nervous system- NAD
P/A- MILD TENDERNESS PRESENT
A - liver abcess 2 to ? amoebic/pyogenic
P-
1. INJ. METROGYL 750MG/IV/TID
2. INJ. MAGNEX FORTE 1.5MG/IV/BD
3. INJ. PAN 40MG/IV/OD
4. INJ. OPTINEURON 1 AMP IN 100ML NS/IV/ OVER 30 MIN
5. INJ. TRAMADOL 100MG IN 100ML NS/IV/OVER 30MIN/ SOS
6. INJ. THIAMINE 1AMP IN 100ML NS IV/OD
Day 3
S - pain abdomen decreased compared to yesterday
No fever spikes
O - on examination
Patient is concious, coherent
Icterus- present
Vitals-
Temperature- 98.6
Pulse rate- 96
Blood pressure- 110/70
Respiratory rate- 20
Spo2- 98% at room air
Systemic examination-
Cardiovascular system- S1 and S2 heard, no murmurs
Respiratory system- bilateral air entry present, normal vesicular breath sounds
Central nervous system- NAD
P/A- MILD TENDERNESS PRESENT
A - liver abcess 2 to ? amoebic/pyogenic
P-
1. INJ. METROGYL 750MG/IV/TID
2. INJ. MAGNEX FORTE 1.5MG/IV/BD
3. INJ. PAN 40MG/IV/BD
4. INJ. THIAMINE 1 AMP IN 100ML NS/IV/ OD OVER 30 MIN
5. INJ. TRAMADOL 1 AMP IN 100ML NS/IV/OVER 30MIN/ SOS
6. INJ. DICLOFENAC 3ML=75MG IM/BD
7. TAB. PCM 650 MG PO/QID
8. INJ. NEOMOL 1G IV/SOS
DAY-4
S- pain abdomen increased, SOB increased
O - tenderness and rigidity decreased when compared to presentation. Vitals stable, RR 24cpm, review ultrasound shows 40-50% liquifaction with mild free fluid
A - amoebic / pyogenic Liver abcess
P- pain management with Tramadol, IV fluids, Gen surgery review.











Comments
Post a Comment