MEDICINE CASE DISCUSSION
This is an E-log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence-based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed .
I have been given this case, in an attempt to solve and understand the topic of "Patient's clinical data analysis”. This has helped me develop my competency in reading and comprehending clinical data including history taking, clinical findings and investigations. The goal is to come up with a diagnosis and treatment plan.
PAVITRA BALDAWA
ROLL NO-104
20TH NOV 2021
65 year old female with complaints of swelling of lower limbs, Shortness Of Breath and decreased urination.
I've been given this case to solve, in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data - including history, clinical findings, investigations - and come up with diagnosis and treatment plan.
Following is a brief about the case,
(History as per date of admission).
CHIEF COMPLAINTS:
A 65 year old Female, resident of Nalgonda and home-maker by occupation, came to Medicine OPD on 15/11/2021 with chief complaints of
• Pedal Edema since 3 months
• Shortness of breath since 1 week
• Reduced urine output since 1 week
• Fever since 4 days.
HISTORY OF PRESENT ILLNESS:
The patient was apparently asymptomatic 3 months ago, when she developed Pedal Edema that was insidious in onset, gradually progressive.
It was associated with Shortness of breath on exertion since 1 week. She later had similar complaints during rest(MMRC grade 4). It had no aggrevating or relieving factors.
It was also associated with decreased urine output since 1 week.
She developed fever 4 days ago that was sudden
in onset, non progressive. There were no aggrevating factors and was relieved on medication.
No history of :
• Vomiting
• Pain abdomen
• Loose stools
• Palpitation
• Chest pain
PAST HISTORY:
• She was diagnosed with chronic kidney disease 6 years ago, for which dialysis was done 4 times, until 4 years ago.
There was lack of follow up visits.
Has been on conservative medications since then.
• She was also diagnosed with hypertension for which she is on medication
• No history of DM, TB, Asthma, Epilepsy.
• No history of surgery in the past.
PERSONAL HISTORY:
- Bowel and Bladder - Reduced urine output
- Addictions- tobacco chewing since 40 years.
FAMILY HISTORY:
In this case it is insignificant.
GENERAL EXAMINATION:
The patient is conscious,coherent and cooperative; well oriented to time,place and person.
She is sitting comfortably on the bed.
She is moderately build and well nourished.
- Edema - pitting type present.
Vitals:
- Pulse rate - 70 beats per minute
- Respiratory rate - 20 cycles per minute
- Blood pressure (left arm) - 110/70 mm of Hg
SYSTEMIC EXAMINATION:
CVS: S1 and S2 heard. No added thrills or murmurs heard
RESPIRATORY SYSTEM:
Normal vesicular breath sounds heard.
ABDOMEN:
Soft and non-tender.
No organomegaly seen.
CNS:
Conscious and coherent.
Normal sensory and motor responses.
INVESTIGATIONS:
Investigations ordered are : CBP, RBS, RFT, ECG and USG.
Hemogram:
- Interpretation - NORMOCYTIC NORMOCHROMIC ANEMIA WITH RELATIVE NEUTROPHILIA.
RBS: 160 mg/dl
RFT:
- Serum Creatinine: 5.1 mg/dl
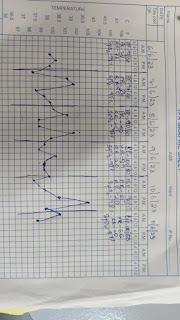
ECG
USG :
PROVISIONAL DIAGNOSIS:
The patient is suffering from chronic kidney disease and is now on maintenance dialysis.
TREATMENT:
• Supportive care is given and patient maintained on hemodialysis
• Salt restriction < 2gm/day
• Fluid restriction < 1.5 L/day.
NOTES :The patient was advised to get dialysis done on a regular basis (atleast 10 more cycles).
• If any puffiness encountered, asked to come to hospital immediately.






Comments
Post a Comment